Begin your evaluation with identifying any “red flags” to determine if the patient needs to be referred to a physician or is non-orthopedic related.
Red Flags:
- Night or waking pain
- Neurologic symptoms
- Fevers or chills
Use the following special tests to determine a specific diagnosis:
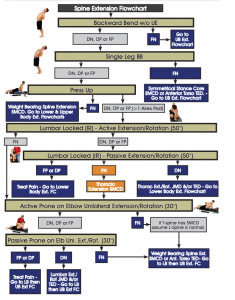
- Multi-segmental extension/flexion functional assessment
- Dx with Extension: Spondylopathy
- Dx with Flexion: Disc
- Stork Test & Quadrant Test
- Dx: Facet Dysfunction
- SLR & Wells SLR
- Dx: Disc pathology
- Thigh Thrust
- Dx: SIJD
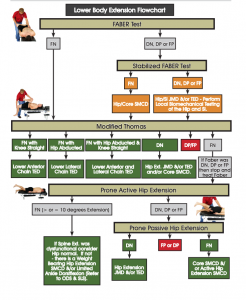
- FABER, FADIR & Posterior Pelvic Pain Test (PPPT)
- Dx: Referral from hip
- Prone Instability Test & Passive Lumbar Extension
- Dx: Lumbar instability
- Palpation of Spinal Muscles
- Dx: Erector Spinae, QL Injury
If you can’t determine a specific dx OR if you can’t figure out how to proceed, move on to TBCS below.
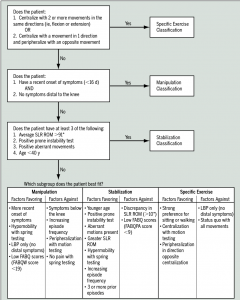
The Treatment Based Classification System
Consists of 4 different classification categories:
- Manipulation
- Specific Exercise (Flexion, extension, and lateral-shift patterns)
- Stabilization
- Traction
Manipulation
- Current symptom duration of less than 16 days
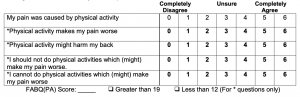
- Score of less than 19 on the Fear-Avoidance Beliefs Questionnaire
- Hypomobility of lumbar spine assessed with PA pressure
- IR of at least one hip greater than 35º
- Symptoms that do not extend distal to the knee
With 4/5 of the above factors, the likelihood of improvement with manipulation is greater.
Stabilization
- Less than 40 y.o.
- an average SLR ROM greater than 91º
- Aberrant movements during lumbar flexion and extension ROM
- (+) Prone Instability Test
- Hypermobility with Spring testing
- Increase in frequency of LBP episodes
- 3 or more prior LBP episodes
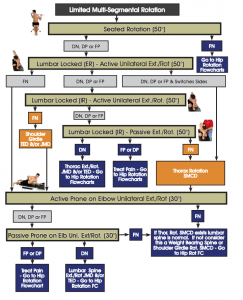
Specific-Exercise
Centralization is defined as occurring when a movement or position results in the absence of p! or parasthesia, or causes migration of symptoms from an area more distal or lateral in the buttocks an/or LE to a location that is more proximal to the midline of the Lumbar spine. Directional preference goes hand in hand most often, meaning that movement in one direction improves pain and symptoms while movement in the opposite direction worsens pain and symptoms.
- Patient has a strong preference for sitting or walking
- Centralization with 2 or more movements in the same directions
- Centralization with a movement in 1 direction and peripheralization with an opposite movement
Traction
- Presence of LE S&S of nerve root compression (i.e. parasthesia, weakness, etc)
- Absence of centralization with movement testing
Interventions for Classification Categories
MAnipulation
- Manipulation of the lumbopelvic region
- AROM exercises
Stabilization
- Promoting isolated contraction and co-contraction of deep stabilizers (Multifidus, TA)
- Strengthening of large spinal stabilizers (Erector Spinae, Oblique Abdominals)
Specific Exercise
Extension
- End-range extension exercises
- Mobilization to promote extension
- Avoidance of flexion activities
Flexion
- Mobilization or manipulation of the spine and/or LE
- Exercise to address impairments of strength or flexibility
- Body weight-supported treadmill ambulation
Lateral Shift
- Exercises to correct lateral shift
- Mechanical or autotraction
Traction
- Mechanical or autotraction
Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007; 37(6):290-302. doi:10.2519/jospt.2007.2498
